Introduction
Majority of patients undergoing decompressive craniectomy (DC) for traumatic brain injury may develop post-traumatic hydrocephalus (PTH). This remains a challenge to manage as most patients are tracheotomised and run high risk of shunt infection and malfunction following VP shunt. Theco-peritoneal shunt (TP shunt) may be an attractive alternative in this scenario.
Aims & Objectives
To assess the role of TP shunt in PTH with respect to the patient population, complications & clinical outcome in TBI.
Materials & Methods
In this retrospective study over 32 months (September 2009–April 2012) records of all patients of TBI who underwent TP shunt at a level 1 trauma centre were analysed. Clinical, radiological and follow up data were reviewed in all cases.
Observations & Results
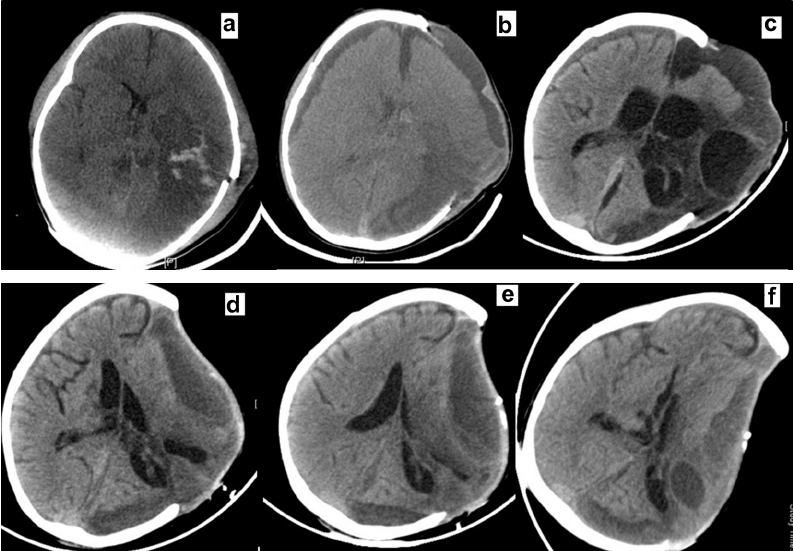
A total of 22 TP shunts were done in the study period. Of these 77.2% patients had severe head injury, 18.2% had moderate head injury and 4.5% had mild head injury. The most common initial CT findings were acute SDH in 86.4% and contusions in 81.8% of the patients. 95.5% patients underwent DC at initial admission. Most common presentations of PTH were bulging flap (95.5%), vomiting (72.7%) and headache (63.3%).
91.9% of the patient had tracheostomy in situ. Of these, 5 patients (25%) had positive tracheal cultures and six (27.3%) patients had scalp bedsore/flap infection prior to TP shunt. Following TP shunt, 77.3% patients showed clinical &/or radiological improvement. Shunt infection and revision rates were 0% and 22.7% respectively.
Conclusions
PTH in patients with TBI needs a holistic approach in view of scalp bed sores, tracheostomy and altered ventricular anatomy. TP shunt is a safe, minimally morbid procedure which should be considered as an attractive alternative to VP shunt in patients with PTH.